9 Steps to Strong Bones: Taking calcium supplements is NOT one of them.
Posted on December 21, 2015 by Dr. G
Bone health is quickly becoming a concern for more and more people. Of course, with our aging population of baby boomers, the number of people who will suffer the brittle bone disease of osteoporosis is going to skyrocket, making hip replacements and orthopedic surgery a very busy and expensive profession. And just like everything else in healthcare, bone health is becoming less black and white. People are suffering more and more with little hope for healthy options to prevent the high cost of diseases like osteoporosis.
It is no longer simply about adequate calcium ingestion (actually, it never was; that was just successful marketing by the dairy industry). We’ve limited our attention to bone health to include only osteoporosis and the reduction of bone density. If you think the only people who have to consider bone health are menopausal women, you are sadly mistaken. New research is opening our eyes to more of what impacts bone health and total health. Everyone should pay attention to this because chances are that you may be one of the people at risk for bone health issues. Our bones are incredibly complex organs, just as complicated as any other system in the body.
A recurring theme in my writing is the fact that we must expand our knowledge of how our body expresses health. This is because we live in a time where the number of environmental factors that interfere with us living a healthy life, which should be innately possible without any knowledge or intervention, is reaching a point of critical concern.
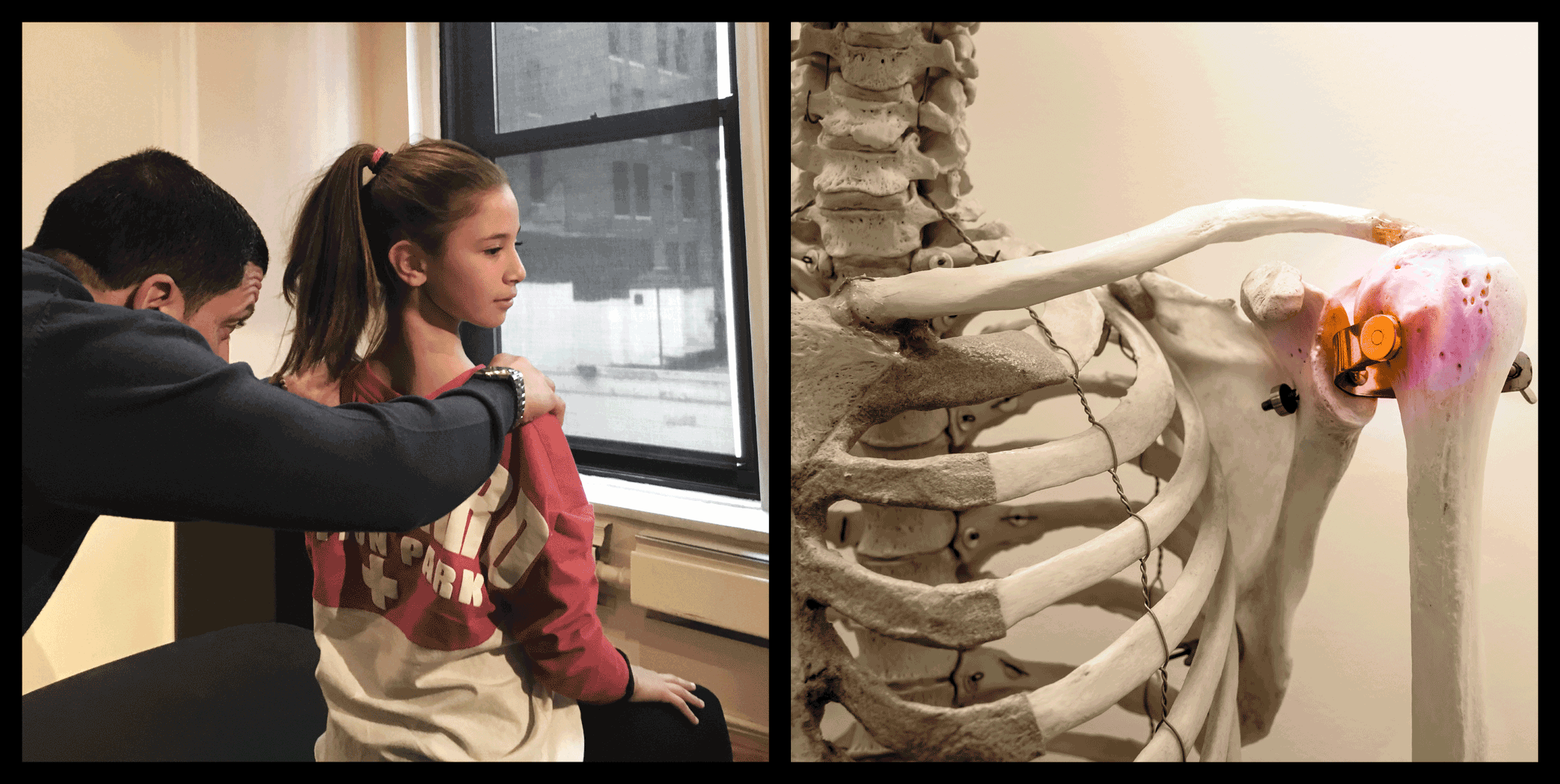
Our bones are responsible for so many seemingly unrelated functions. They provide critical feedback to our brain and nervous system, they help to regulate scores of hormones, and they are factories for our immune and blood cells. Therefore it stands to reason that diseases of bone like osteoporosis have consequences beyond brittle bones. This is why it is so important for your doctor to be a holistic doctor because looking at a singular symptom of poor bone health, like low bone-mineral density (brittle bones), is terribly short sighted and allows many other health conditions to progress.
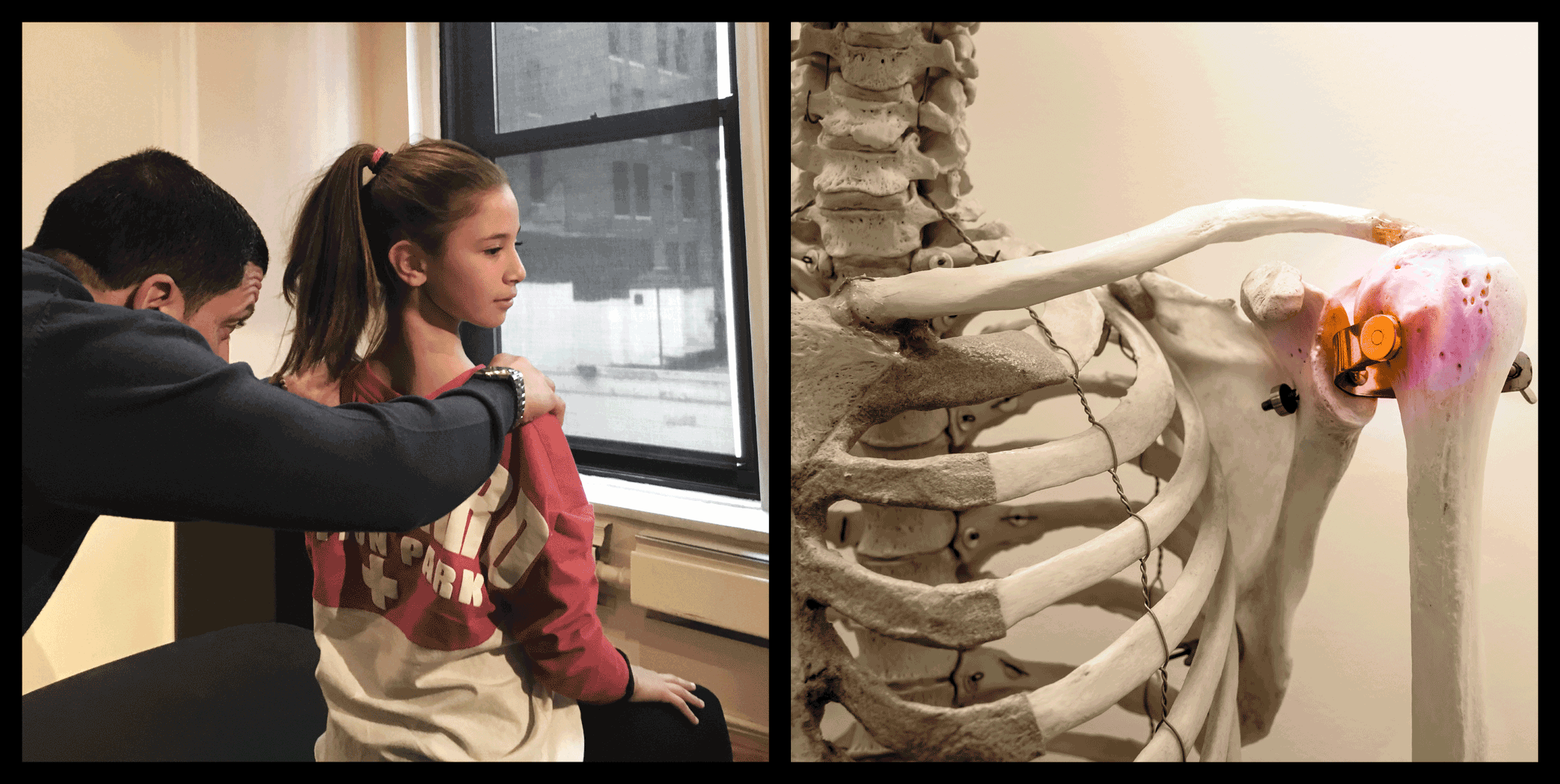
Bone health begins at birth and never stops until you die. Waiting until you are 60 years old and diagnosed with low bone density before you take action or consider bone health is like waiting for your first heart attack before you consider your heart health. It’s stupid and it is what most people do.
Bone health contributes to many things, from sports injuries from the young athletes on the travel soccer team to the middle-aged weekend warrior. Some examples:
- Scoliosis
- Chronic joint pain
- Shin splints
- Sever’s disorder of the heel and osgood schlatters of the knee (apophysitis)
- Recurring injuries
Here are some little known facts about bone health.
- Hormones that regulate energy production and hunger, such as leptin, play a major role in bone health. Leptin resistance is a condition of abnormal energy production and storage that is seen in our modern world.
- Decreased progesterone in all ages contributes to bone loss. This is often not considered until menopause, but progesterone levels can actually be negatively impacted throughout your life.
- DNA transcription factors found in the gut and impacted by diet directly impact the differentiation of cells in our bone to become osteoblasts and osteoclasts. The cells responsible for laying down new bone and remodeling bone. Linking gut health and bone health.
- Bone health is directly impacted by the interplay of several key hormones, all of which requires LDL cholesterol for their production. There is a link between taking statin drugs and poor bone health.
- Osteocalcin is a hormone produced by our osteoblasts and is involved in creating insulin sensitivity. Insulin sensitivity is the opposite of the pre-diabetic state of insulin resistance. Osteocalcin also helps us to make more testosterone, which improves bone health in both men and women.
- Vitamin K2 and the hormone osteocalcin together are involved with where and how calcium can be deposited in bone, teeth and even arteries. K2 is deficient in our culture due to its loss when processing food. When there is a deficiency of vitamin K2, calcium loses its ability to go where it is needed and may result in calcium being deposited where it is not needed and result in conditions like heart disease.
- Osteocalcin needs to be activated by a process of adding a carboxyl group. Carboxylation of osteocalcin is inhibited by insulin resistance and diabetes. This explains the increased risk of osteoporosis for diabetics. The interplay of vitamin K2, blood sugar/insulin regulation and osteocalcin carboxylation make it difficult to do a simple blood test. A clinical picture must be drawn that is based on many factors, including blood markers, history, lifestyle and genetics.
- Your arterial calcium index score can be an indicator of poor vitamin K2 levels and osteocalcin physiology. This, however, is an x-ray-dependent diagnostic test and should be limited to those who are at high risk for existing heart disease. X-ray exposure should be limited as much as possible because it is ionizing radiation.
- According to Dr. Jack Kruse, calcium can also be deposited in teeth as plaque. This may be a better indication of vitamin K2 deficiency and poor activation of osteocalcin. A dental hygienist or a good look at your own teeth can help you determine if you are vitamin K2 deficient and at risk for depositing calcium in blood vessels that leads to heart disease.
- Vitamin K2 is present in unprocessed foods. Organic green leafy vegetables have vitamin K2, but produce that is exposed to pesticides is depleted of vitamin K2. Vitamin K2 is indirectly produced in our bodies by the bacteria present in our gut, if our gut is healthy. Poor gut health and microbiome can be another indicator of poor Vitamin K2 levels.
- Exercise can be helpful, but the positive effect of exercise is supposed to have can be prevented due to leptin resistance caused by the standard american diet (SAD).
Poor bone health does not cause diseases like atherosclerosis, diabetes, heart valve disease, immune challenges, and sleeping disorders. Rather, poor bone density and health are valuable indicators for a dramatically increased risk of all these conditions.
Routine Blood Tests provide a wealth of clinical information.
- Comprehensive Metabolic Panel. Provides liver function markers including alkaline phosphatase, LDH, GGT.
- Complete Blood Count. Should be included in all routine blood tests because of its very low cost and very high diagnostic value.
- Vitamin D (25 hydroxy). At a minimum, this number should be above 50. 80-100 is optimal.
- High Sensitivity C- reactive protein (HsCRP). Inflammatory marker that correlates closely with inflammatory cytokines like TNF-alpha and IL6 (which closely correlate with leptin resistance).
- Hemoglobin A1C. 3 month running average for blood sugar. Very important in determining insulin resistance.
- DHEA Sulfate. Low DHEA also correlates with cortisol dysrhythmia. DHEA is a necessary precursor to the very important hormones for bone density, progesterone and testosterone.
- Lipid Panel. To include total cholesterol, HDL, LDL, triglycerides, oxidized LDL, oxidized HDL (further evidence of inflammatory up-regulation and the ability or inability for the liver to effectively remove systemic inflammation.
- Total & Free Testosterone. Sometimes a total testosterone number is normal or optimal, but the non-protein bound active free form may be low. Checking both is important.
- IGF-1 (Insulin like growth factor-1). Correlates with growth hormone levels. Ideally this number should be above 100.
The best steps you can take to begin to improve bone health:
- Reduce leptin resistance with a paleo style diet that focuses on fresh organic vegetables, raw nuts and seeds, pastured eggs (from chickens not fed soy), healthy meats and healthy animal fats like EPA and DHA (animal source Omega 3 fat).
- Avoid dairy. Yes, that’s right, I said avoid dairy. That includes all forms of non-raw pasteurized dairy products.
- Vitamin D. Keep vitamin D levels over 50 on blood tests. Supplements vitamin D3 regardless of your blood levels at a minimum of 5000 i.u. per day.
- Vitamin K2 at 50-150 mcg per day.
- Control gut inflammation.
- Practice intermittent fasting. Fasting is a great way to temporarily decrease the antigenic load in the gut where 85% of the immune activity resides. Fasting shuts down much of our inflammatory processes. There are many forms of intermittent fasting. Please feel to inquire about the types available to you in the comments section.
- Gut inflammation is further inhibited by supplementing L-glutamine and DGL regularly, especially if you are aware the gut dysfunction is a part of your health history. L-glutamine and anti inflammatory effect can be experienced with regular consumption of bone broth.
- No calcium supplementation. If you have a diet rich in whole, healthy foods, please do not supplement calcium. This has been shown to lead to adverse outcomes for reasons discussed above.
- Regular intake of liposomal turmeric and resveratrol to regulate inflammatory cytokines, increase IGF-1 and at the same time (in the case of resveratrol) increase bone density and decrease bone resorption.
- Increasing neuronal and endothelial nitric oxide synthase (eNOS) and decreasing inducible nitric oxide synthase (iNOS) with exercise and L-Arginine supplementation. iNOS will contribute to proinflammatory processes and bone loss, whereas eNOS will contribute to increased bone density.
- Sleep Hygiene. Sleep is critical to total health, recovery and healing. Addressing issues that interfere with sleep is essential.
Thanks for reading!
What are your thoughts on bone health? Share your stories and comments below!





