From raging to a trickle: The Hormone Story
Posted on August 24, 2015 by Dr. G
Here is a question from a dear friend of over 30 years, Meredith: “I am thinking about bio-identical hormone replacement therapy (BHRT), not for symptoms of menopause, which seems to be starting early for me because I can deal with that, but rather, I have a pretty significant family history of cancer and other diseases, and I hear that BHRT can be good for me. I want to do what’s best for my longevity and do what’s best to make sure I am around to raise my young children.”
Meredith, 45, lives a healthy lifestyle with reasonable and mostly healthy exercise and dietary habits. She has been known to party hard every once in a while and indulge in less-than-healthy activities, but this is increasingly rare and nothing like it was 20 years ago. As we learn more about genetics and disease, more and more people, mostly women, are faced with tough decisions, like prophylactic bilateral mastectomy (which has received increased awareness lately because of a decision made by celebrity Angelina Jolie).
The question related to BHRT can be very different for many people. Questions I get often on the subject are related specifically to reducing the symptoms of menopause, either naturally occurring or surgically induced, each of which have different considerations. The questions are sometimes related to improving libido, reducing the dryness and pain associated with intercourse after menopause. Or many people have a family history of cancer that may or may not be related to estrogen receptors.
Patients and subscribers to our website ask me these questions because they know I am not a gynecologist or a primary care physician. They ask me because they know my expertise is in functional medicine and optimal health restoration. Most people who are asking my opinion already have been given an opinion by their gynecologist or primary care physician.
Here are some of the basics when educating my patients about hormones.
1. Hormones have a significant amount of interplay. There are more than 600 hormones in the human body, and they are all interrelated in a complex web. Like a spider’s web, it is impossible to touch any part of the web without moving the entire web and therefore affecting systems that are seemingly unrelated. Estrogen or any other hormone replacement therapy does exactly that – it interferes with the complex interplay of all hormones.
An example of this web-like interplay is when a poor diet and lack of exercise can cause dysglycemia (abnormal regulation of blood sugar), which over time, disrupts the concentrations of hormones that regulate blood sugar, such as insulin and cortisol. This disruption of two important hormones over a long enough period of time will alter brain chemistry, which will alter messages given to the chief gland in the body, the pituitary, which will impact hormones from the thyroid, pancreas, ovaries, and others, resulting in a common condition called PCOS (polycystic ovarian syndrome), which is the No. 1 cause of infertility in the United States. PCOS is 100 percent reversible, naturally, without drugs or hormone therapy.
2. Trace hormone production occurs after menopause. While hormone production by the ovaries diminishes after menopause, there is supposed to be trace production of the very same sex hormones (progesterone, testosterone, and estrogen) by the adrenal glands, two triangular organs that sit on top of each kidney.
The adrenal glands play a very important role in managing all types of stress in the body as well as blood pressure and blood sugar. The sex hormone production by the adrenal glands is overshadowed by the larger amount produced by the ovaries (or testes in men); therefore, their contribution is easily overlooked. After menopause, however, when the ovaries cease to produce sex hormones, the sex hormones produced by the adrenals can become the producer of enough sex hormone to silence the symptoms associated with menopause, osteoporosis, and any other manifestations of the complex web they contribute to.
There are indigenous societies around the world (usually in third world nations) whose languages do not have words to describe symptoms associated with menopause because there are no symptoms associated with menopause. I know that doesn’t help much because none of us want to live in a hunter-gatherer culture in the Amazon, but there is a lot to be learned from that little factoid.
Understanding the impact our first world industrialized lifestyle has on our adrenal function and then trying to improve it naturally is a common area of study and practice in functional medicine.
3. Do not overlook the brain. Nerves from the brain can do one of three things: 1, communicate with another nerve; 2, cause a muscle to contract; or 3, cause a gland to secrete. Hormones are secreted by glands. The gland does not make decisions; the nervous system (brain) does based on the internal and external environment of the body.
Health practitioners of all types, including functional medicine doctors, too often rely on the idea that a gland can “fatigue.” Glands do not “fatigue,” but the effect can be as if they have. It seems like semantics, but it is not. If the focus is on the gland fatiguing, then all of the support will be to supplement the gland with the nutritional precursors and/or “adaptogens” they need for the adrenal glands to produce adequate hormones.
Unfortunately, little attention is paid by practitioners on the possible brain and neurological mechanisms that would prevent various glands from producing the requisite level of hormones even with the presence of adequate precursors.
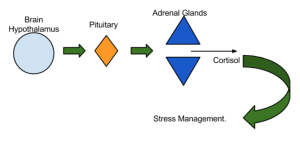
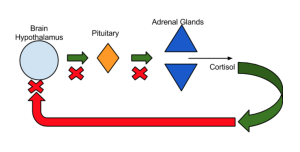
For example, a well known anatomical pathway from the brain to the adrenal glands is from an area of the temporal lobe called the hypothalamus, which projects a message to the pituitary gland, which then projects a message to the adrenal glands telling them to secrete their products (hormones).
This system has a negative feedback loop, which means that if there is too much cortisol produced because of a chronic form of stress (physical, chemical, immunological, mental), then the cortisol actually shuts down the cells in the hypothalamus (brain), preventing them from perpetuating the same pathway (see below). This protects us from the danger of overproduction of hormones.
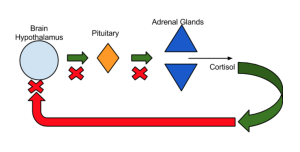
Its a very smart system in acute situations; however, this system has unintended consequences when it becomes chronic. One of those unintended consequences is a decreased production of all adrenal hormone activity. Even if you remove the stress, and no longer have the stressor, the effect on the hypothalamus portion of the temporal lobe could be long-term atrophy. This has been shown repeatedly in studies. There are natural ways to improve hypothalamic activity and protect this very important part of the brain, especially because it is also implicated in memory and is one of the major areas of study for Alzheimer’s disease. Simple compounds like phosphatidylserine in the right formulation can be of great use in supporting this most important part of the brain and its relationship to adrenal function and hormone health.
4. The immune system plays a role in hormone health indirectly and directly. I mentioned above that chronic stress can impact adrenal function and therefore affect brain pathways that regulate all hormones, including sex hormones. You might say or think that you don’t really have a lot of “stress.” You have good relationships, money is not a problem, and life is overall pretty good; therefore, the conclusion is, “I cannot be overstressed because life is good.” Not so fast.
Let’s take a minute to talk about stress. There are several types:
- Acute, external life-threatening stress. The ultimate example of acute stress is being chased by a lion, resulting in a massive stress response in a very short-lived period of time.
- Chronic external mental stress. Chronic stress can include being in a bad relationship, hating your job, money worries, etc., which are lower levels of stress than the lion chasing you but can be chronic and therefore be a major challenge because the situation can last months, years, or decades.
- Acute internal stress (chemical/immunological). When a flu virus enters the body, it’s kind of like a microscopic “lion,” requiring a massive protective response. It is a massive response that is relatively short-lived, 5 to 7 days, and then you recover and go back to normal. Like fighting or running away from the lion, fighting a virus uses a massive amount of energy and resources.
- Chronic internal stress (chemical/immunological). What if the immune system had to fight a virus all day every day without rest? You would get fatigued, and the body systems we have to adapt would “fatigue,” just like they do with chronic stress associated with a bad marriage, money issues, and the like.
This type of chronic immune stress is very common today. Millions of Americans have immune responses that are relentless in the form of food sensitivities they should not have or autoimmune conditions they should not have. These are often present for years without detection, resulting in a failure, or “fatigue,” of our ability to adapt. They then result in countless possibilities for symptoms, including hormone imbalances.
5. Toxicity. The human body is genetically adapted to detoxify us from the byproducts of our own metabolism. Organs such as the GI tract, liver, kidneys, and sweat glands are perfectly suited to detoxify us from a world that was meant to be 100 percent organic and non-polluted. After all, humans have adapted over millions of years. Only the last couple of hundred years and mostly the last 60 years have produced a level of pollution and toxicity we have never seen before (and are therefore not adapted to handle genetically).
In addition to detoxifying us from our own waste, used up hormones, insect bites, and the like, we have to detoxify from chemical pollutants in the air, additives to our processed food, the chemicals off-gassing around us (for instance, that new car smell), volatile organic compounds in building materials, medications, and countless other modern insults. Toxicity creates a similar type of silent stress as the immune stress discussed above. Many of the chemicals we discussed are classified as endocrine disruptors (the endocrine system is the hormonal system) – chemicals that alter the hormone system due to exposure.
Taking all of the above considerations into account is the first step when helping people make decisions about BHRT. They must all be addressed. If you decide to move forward with BHRT, addressing the above can ensure that you benefit optimally. If you decide not to move forward with BHRT, it may be because the above steps made the decision unnecessary because the symptoms are gone, and health is restored. It all depends on your history, pre-existing state of health, previous exposures to endocrine challenges, etc.
Dispel the myths about hormone replacement therapy: Know the facts
1. Bio-identical hormones are “natural” and “identical” to our own.
The hormones exist naturally in plants like soy and in the body fluids of mammals. If you eat the soy plant in massive quantities or drink the horse’s urine, you may get “natural” hormones. If not, and I know Meredith is not interested in either of those two choices, then you will not get “natural” hormones. Soy has all kinds of other issues to consider. I personally avoid soy and not just because I am a man.
Large companies have factories that extract the hormone molecules with a complicated chemical process to bring them from their source, the soy plant and the horse urine, to the final spray, cream, pill, or lotion. The companies that do this sell their product equally to compounding pharmacies (that make bio-identical hormone products not under FDA-approved rules for dosage and marketing) and large traditional pharmaceutical companies that make FDA-approved traditional medicine.
Put simply, the Estradiol in the FDA-approved drug and the “bio-identical” cream are identical. The compounding pharmacies and traditional pharmaceutical companies are using the same product from the same place. Therefore, the terms “natural” and “identical” are marketing terms used by ad agencies and exploited by companies that convince celebrities like Oprah and Suzanne Somers that there is something more natural and safe about them, which brings me to the next myth.
2. Bio-identical hormones are safer than traditional pharmaceutical products. This is a claim made by the “bio-identical” industry because they are not regulated by the FDA and therefore do not go by the same rules as traditional pharmaceutical companies. I am not interested in protecting the pharmaceutical industry; on the contrary. I know that the fewer drugs people take, the healthier we all will be. However, that does not mean I want to perpetuate myths.
Bio-identical hormones are produced by large compounding pharmacies. They chemically prepare their products in a way that is not predictable. Each batch will have varying doses of hormone. FDA-approved medications are required to have their doses be exact in each preparation; therefore, they are more predictable, and some would say that it’s safer to be more predictable. FDA-approved preparations must disclose the benefits and the risks according to federal law, which we know is imperfect, to say the least, but the compounding pharmacies are not held to any such standard.
Bio-identical hormones have been approved for use only because of their ability to decrease symptoms of menopause and prevent osteoporosis, same as the traditional medications. All other claims are marketing claims.
3. Hormone testing with either blood or saliva can determine the safe dose needed for the doctor to prescribe. Menopausal women have, by definition, “abnormal” hormone levels relative to their youth because they are going through a natural process called menopause. These levels change by the hour, and a blood or saliva test gives a snapshot in time and is therefore unreliable for prescribing.
4. The “weak” form of estrogen called “Estriol” found in bio-identical preparations is safer and has been shown to prevent or reverse breast cancer. Another myth; there are no human studies to show this.
5. Bio-identical hormones can help reduce the incidence of certain cancers and other diseases. For reasons stated above, there is no reason to believe that the benefits and risk experienced by the FDA-approved drugs would be any different. Long-term studies on bio-identicals have not been performed; therefore, claims they do things their “identical” counterparts (FDA-approved drugs) don’t are not reliable. The only benefits the FDA attributes to menopausal hormone replacement therapy is reduction in age-related bone loss and decreasing the hot flashes and symptoms of menopause. Their risks, however, are to the contrary of the claims that diseases can be prevented with BHRT. Large studies show that cancer increases with hormone replacement therapy. As a matter of fact, in the 1970s and ’80s, the biggest of the blockbuster drugs was premarin, which was shown to cause breast cancer. When the news about this was released, there was a dramatic decrease in the use of premarin, and that decrease resulted in the only downward trend in breast cancer statistics to occur in the last 40 years.
Again, because the hormone is the same in bio-identical hormones, there is no reason to believe the risks are different. “In fact, like FDA-approved MHT drugs, they may increase the risk of heart disease, breast cancer, and dementia in some women. (See www.nhlbi.nih.gov/whi/index.html for information on the Women’s Health Initiative, a large, long-term study that tested the effects of FDA-approved MHT drugs.) No large, long-term study has been done to determine the adverse effects of ‘bio-identical’ hormones.”
But some data suggest that estrogen can decrease the risk of heart disease when taken early in postmenopausal years. If you are going to eat the Standard American Diet, not exercise, and not learn what your specific needs are to be healthy, then the decision to use hormones to combat heart disease is yours. Something has to kill you. I hate to sound so cold, but there is enough evidence to show that heart disease is a lifestyle disease and not caused by too little estrogen replacement therapy. No need to waste more time on this point.
It’s funny, though; the same reference for the statement above about reducing heart disease, makes this statement:
“In the largest clinical trial to date, a combination estrogen-progestin pill (Prempro) increased the risk of certain serious conditions, including:
- Heart disease
- Stroke
- Blood clots
- Breast cancer
Osteoporosis is a disease that has many potential factors. There is evidence now that osteoporosis has to be evaluated, not as being caused by a singular chemical in the body that can be replaced, like Estrogen, but rather a complex interplay between hormones, digestion, inflammation, immune function (autoimmunity), micronutrients, the microbiome (bacteria), and more. Prescribing hormone replacement therapy and calcium supplements is denying the existence of many factors that can be influenced naturally by lifestyle and/or nutraceutical use. I believe this approach to be irresponsible.
There is so much to discuss. I believe this is a good start. Every case is unique, which makes your decision a very personal one.
Thanks for reading!
There are no right and wrong decisions. Decisions are made on a spectrum that weighs risks and benefits.
Please share with us in the comments section below your unique story as it relates to hormone replacement therapy, whether you decided for or against it, bio-identical or not. Your story can be very helpful to people just like you who are making a tough decision.





