Cortisol Face: Understanding the Link Between Stress, Insulin Resistance, and Your Health
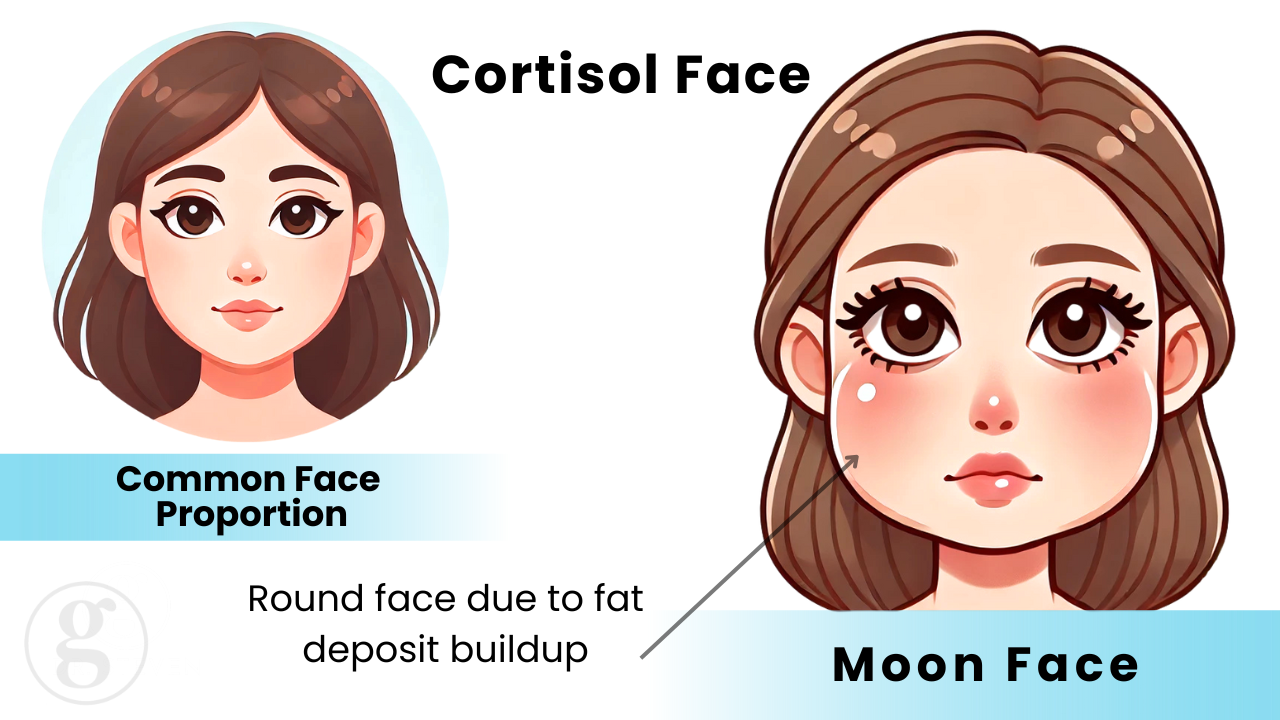
In the world of functional health and nutrition, we’re constantly uncovering new connections between our lifestyle choices and our health. One intriguing phenomenon that’s gained attention in recent years is what we call “cortisol face.” This condition, once known as “moon face” in medical circles, has a fascinating history and important implications for our modern lifestyles.
The Origins of Cortisol Face
When I was in school thirty years ago, doctors learned about a rare condition called Cushing syndrome, which affected only about 10 in a million people¹. This syndrome, typically caused by a tumor in the pituitary gland, excessive steroid use, or certain cancers, resulted in distinctive facial puffiness along with other symptoms like depression, central obesity, and fatigue².
Beyond Cushing Syndrome: A Modern Epidemic?

While true Cushing syndrome remains rare, we’re now seeing a rise in what we might call “Cushing-like” symptoms in the general population. This raises an important question: Could elevated cortisol levels be affecting more people than we realize?
The answer, it seems, is yes. Many individuals are experiencing symptoms reminiscent of Cushing syndrome, including:
- Facial puffiness
- Fatigue
- Depression
- Central obesity
However, the cause isn’t necessarily autoimmunity, a tumor or medication. Instead, it’s often linked to our modern lifestyles³.
The Cortisol Connection
Cortisol is often labeled as the “stress hormone,” but its role in our bodies is far more complex. It’s also a crucial player in:
- Blood sugar regulation
- Sleep-wake cycles
- Immune function
When cortisol levels are chronically elevated, it can lead to a host of health issues, including the symptoms we associate with “cortisol face”⁴.
The Insulin Resistance Factor
While stress is certainly a contributor to elevated cortisol, there’s another key player that often goes overlooked: insulin resistance. Insulin resistance can trigger a cascade of hormonal imbalances, including increased cortisol production⁵.
This connection between insulin and cortisol highlights the intricate dance of our endocrine system and underscores the importance of addressing root causes rather than just symptoms and for the clinician to understand the ‘web of physiology’. This refers to the idea that influencing one aspect of physiology will have an effect on many.
Beyond Supplements: Addressing the Root Cause

It’s tempting to reach for ‘cortisol-reducing’ supplements when faced with these symptoms. However, it’s crucial to remember that we can’t out-supplement a poor lifestyle. True healing comes from addressing the underlying issues.
To effectively manage cortisol levels and reduce “cortisol face,” consider:
- Improving insulin sensitivity through diet and exercise
- Implementing stress-reduction techniques like meditation or yoga
- Prioritizing quality sleep
- Addressing any underlying health conditions
Conclusion
Understanding the complex interplay between cortisol, insulin, and our overall health is key to addressing issues like “cortisol face.” By focusing on lifestyle factors and addressing root causes, we can work toward balanced cortisol levels and improved overall health.
Remember, your face is often a reflection of your internal health.
References:
- Walker, B. R. (2001). Cortisol–the key player in stress. Endocrinology and Metabolism Clinics of North America, 30(1), 1-14. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11141701/
- Mayo Clinic. (n.d.). Cushing syndrome: Symptoms and causes. Retrieved from https://www.mayoclinic.org/diseases-conditions/cushing-syndrome/symptoms-causes/syc-20351310
- WebMD. (n.d.). What is cortisol? Retrieved from https://www.webmd.com/a-to-z-guides/what-is-cortisol
- Rupa Health. (n.d.). The cortisol-insulin connection: How to manage stress. Retrieved from https://www.rupahealth.com/post/the-cortisol-insulin-connection-how-to-manage-stress
- Medical News Today. (2018). Everything you need to know about cortisol. Retrieved from https://www.medicalnewstoday.com/articles/322335
- Healthline. (2020). 12 Natural ways to lower your cortisol levels. Retrieved from https://www.healthline.com/nutrition/ways-to-lower-cortisol
- Sapolsky, R. M. (2011). Cortisol dysregulation and the development of insulin resistance: Implications for metabolic syndrome. Trends in Endocrinology and Metabolism, 22(2), 101-107. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21432232/
- National Organization for Rare Disorders (NORD). (n.d.). Cushing syndrome. Retrieved from https://rarediseases.org/rare-diseases/cushing-syndrome/
Want to learn more about optimizing your health and longevity? Visit our Blog Home Page for more expert insights. If you’re interested in working directly with Dr. G to see if you’re an ideal client, you can explore more here. Additionally, take a look at Dr. G’s supplement line for products designed to support your metabolic health at Cyrene Labs (Cyrene labs products are only available through licensed providers).