When it come to Lyme and “lyme like diseases”, what you and your doctor don’t know may harm you
Posted on April 10, 2016 by Dr. G
Contradictions in policy and ignorance of research by institutions we are supposed to trust with our health is resulting in misery and suffering.
People suffering chronic symptoms, suffer needlessly. Standards of care determined by political organizations who claim to have public health interests in mind, result in the application of blanket recommendations to individuals regardless of differences in their history, presentation, laboratory findings etc.
There seems to be a lot of attention being paid to the subject of Lyme disease and justifiably so, this is a disease that causes severe chronic suffering and disability. There are more and more people investigating possibilities for diagnosis and treatment.
The reasons for the increased interest is due to:
- A pandemic of chronic symptoms that appears to have an immunological cause.
- The symptoms mimic the symptoms of so many other disorders, especially autoimmune disease, the incidence of which has skyrocketed in recent years.
- Severe contradictions in official policies and science.
It’s this 3rd component I’d like to discuss here.
Lyme disease is associated with a bacterial infection correlated with a bite from an infected tick. This disease was first observed, investigated and named in 1980 when a group of children presented with a specific set of symptoms in and near the town of Lyme Connecticut.
Most of the children affected had a recent history of playing in wooded areas during the warm summer months, having a tick bite, a skin rash, followed by arthritic pain. This is why the attention was turned to the deer tick. There was a clear correlation.
The bacteria is a type called a spirochete. A spirochete is a small spiral shaped bacteria, of which there are different types. Other spirochetes are syphilis, rocky mountain spotted fever.
The contradictions: Policies and myths the perpetuate poor decisions and result in unnecessary suffering and disability.
According to the NIH and the CDC (National Institute of Health and the Center for Disease Control) our major public health institutions for which the medical profession depends on for standards of care and diagnosis, the diagnosis requires:
Policy/Myth: The tick bite must be attached to the body for at least 36 hours to transmit Lyme.
Fact: Not true.
Policy/Myth: Although transmission cannot occur without a tick bite, many people cannot remember being bitten because the deer tick is tiny and the bite is painless.
Fact: less than 20% of confirmed cases of Lyme has a reported history of a 36 hour tick attachment and bite, a rash (erythema migrans) and arthritic symptoms.
Policy Myth: Lyme is endemic to the Northeastern United States.
Fact: Most cases of confirmed Lyme are in the north east however Lyme has been confirmed in all every state as well as Europe, Middle East and Asia.
Policy/Myth: Must have bulls eye rash which is unique to Lyme disease. Although obvious when present and nearly impossible to miss, 20% of cases have no rash.
According to the CDC/NIH, a 2 step process for diagnosis is recommended. First a screening test which is sensitive but often has false positives. “If the screening test is positive, it should be followed by a western blot test which is positive only when a person is infected, thereby confirming the diagnosis”.
The CDC also states that the western blot should not be used alone, since it increases the likelihood of false positives. So on the one hand the western blot does not give false positives and is only positive when infected and on the other hand, it should not be used alone because of false positives.
Tale of two medical societies:
The I.D.S.A. (Infectious Disease Society of America) states Lyme disease is “hard to catch, easy to cure” with a short course of antibiotics. The IDSA claims that a spirochetal infection cannot persist in the body after a short course of antibiotics. The IDSA also denies the existence of “chronic” Lyme disease.
IDSA leaning doctors will treat with short term antibiotics. They are more likely to withhold treatment pending laboratory tests.
I.L.A.D.S. (The International Lyme and Associated Diseases Society) stands in contrast to the IDSA and state that Lyme is difficult to diagnose and treat. This is a more accurate statement, however, it is used as justification for radical treatment approaches based on the presence of “a tick borne disease (not just Lyme) and the patient’s symptoms.
ILADS leaning doctors will make decisions on a case to case basis and are more likely to treat “high risk” bites without evidence of lab testing and will treat with a longer course of antibiotics.
All experts agree that the earlier you treat, the better, since early treatment is often successful. The problem is that a significant portion of those treated with short term antibiotics continue to have significant ongoing symptoms and experts do not agree on the cause of the ongoing symptoms. There is no test available to determine if the course of treatments was effective in eradication of the infection.
The IDSA leaning doctors believe that Lyme symptoms after treatment is not Lyme and represents a post Lyme syndrome, possibly due to autoimmunity and therefore is not responsive to antibiotics. The IDSA essentially regards Lyme as an acute infection, like strep throat, that requires a short term of antibiotics for treatment. These guidelines are now 8 years old and do not reflect current science.
The ILADS leaning doctors believe that ongoing, chronic Lyme symptoms are due to an active infection and therefore requires long term antibiotic treatment until symptoms are resolved. ILADS is more active in updating their guidelines and tend to perform a more exhaustive review of the current literature.
In short, if you are suspected to have Lyme or have confirmed Lyme disease, you may either be treated with a short term of antibiotics, 3-4 weeks or antibiotics for as long as you have symptoms. There are cases that have been on antibiotics for more than 20 years.
ILADS doctors are more likely to investigate the presence of co-infections there is failure to respond to treatment or if the symptoms are relapsing. ILADS doctors also will be more likely to recognized the presence of immune dysfunction, hormone imbalances and opportunistic infections.
May not just be tick bites:
The research now tells us that the spirochete bacteria that causes Lyme can be transmitted from any vector that is known to carry other viruses, bacteria and fungi and can do so at the same time, meaning multiple infections in one bite. These infections can be carried and transmitted by ticks, fleas, mosquitoes. They infect humans and other animals with one single bite. A tick is more likely to be the infective source or vector rather than a mosquito because it lives longer than a mosquito, but that does not mean that it is only the tick that can transmit the bacteria, just less likely to be another source.
Can lyme be sexually transmitted?
This is a question receiving a lot of attention lately. In 1980, the tick borne, northeastern united states, summer month, rash producing disease hypothesis gave us correlation. However, correlation does not mean causation. After all one of the most well known sexually transmitted diseases, syphilis, is a spirochete type bacteria.
Opportunistic infections:
The compromised immune system may show challenges with dealing with common routine infections like Epstein Bar virus (EBV). herpes simplex virus (HSV 1 & 2), HHV6, cytomegalovirus (CMV), etc.
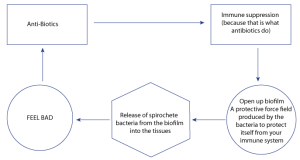
Treatment with antibiotics (especially the long term antibiotics recommended by the ILADS leaning doctors, will lead to the following vicious cycle:
What else do antibiotics do?
In addition to killing bacteria, chronic use of antibiotics (long term use) will also result in opportunistic infections that are not killed by the antibiotic like viruses (viruses are not affected by antibiotics). Due to the immune suppression, the viruses are more likely to burrow deep into our tissues and cells causing damage they would never have caused otherwise.
Neurological symptoms related brain and neuro-lyme must be identified. The recommended short term antibiotic treatment of Lyme with doxycycline antibiotic at 200 mg will never penetrate the brain’s protective barrier called the blood brain barrier (BBB). 400 mg is the dose that will penetrate the BBB, however that is a dose that is likely to induce illness, nausea and vomiting. It has been my experience that many Lyme illiterate doctors do not know this. Ceftin is an antibiotic that does cross the blood brain barrier. Other classifications of antibiotics known as fluoroquinolones like cipro, are known for causing injury and disruption of tendons (not a desired side effect for what should be a young active person).
Antibiotics were discovered in the presence of mold. Well the excessive use of antibiotics will create an environment that is perfect for the growth of mold, resulting in a mold infection.
Co-infections
In New York State (where the study was done, the ticks don’t stop at the border) over 50% of all ticks carry a tick borne disease. Since a single tick bite can simultaneously deliver several bacteria, viruses, fungi or protozoa. 30% of confirmed Lyme cases have 2 or more co-infections. 80% of confirmed Lyme cases have at least one co-infection. These are considered tick borne diseases and they include:
- Babesia
- Bartonella
- Mycoplasma
- Ehrlichia
- Rocky mountain spotted fever
- Anaplasma
- Among others
Co-infections mean that an antibiotic treatment for Lyme may not be helpful in treating for the others. Perhaps the co-infection, under normal circumstances would be a mild self limiting barely noticeable infection like a cold, but under the immune system compromising effects of Lyme, result in chronic ongoing symptoms associated with “post Lyme syndrome”. This is exactly the case with bartonella.
The fact is the aggressive pursuit of identifying co-infections may make sense to get a sense of immune dysregulation and immuno-compromise, so the doctor is aware of your starting point, but the fact is we are likely not aware of nor are we able to test for approximately 80% of would be co-infections.
Identifying bartonella and finding another antibiotic to treat it may not be very wise. The questions that should be asked are:
- Is the immune system dysregulated?
- If so, can anything be done to restore regulation?
These are typically not questions asked or answered by doctors in the 2 medical societies listed above (ISDA and ILADS) even though they may be quite rare “lyme literate” doctors in your community.
It is the role of “lyme literate” functional medicine doctors to understand the immune system and how to naturally support and restore its normal function and doing so in the presence of possible Lyme, other tick borne disease, co-infections, opportunistic infections or autoimmune disease.
Thanks for reading!