Family, Friends & Cancer..
Posted on March 20, 2016 by Dr. G
I am writing this particular post for those whose inner circles are impacted by a diagnosis of cancer, and in case you are wondering, that is or will be all of us. This post actually is applicable to most serious health conditions.
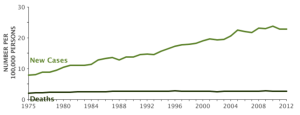
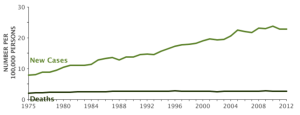
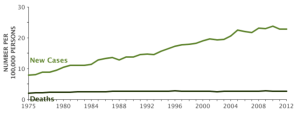
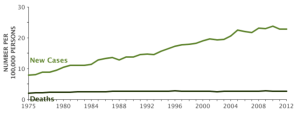
Cancer: An Increasing problem
I hate to say I’ve had a tremendous increase in calls to my office from people recently diagnosed with cancer. There seems to be a contradiction where medical advances are increasing at a rate that is very optimistic and positive in every way, yet the scourge of chronic disease is increasing, not decreasing. As a matter of fact cancer rates are either increasing in younger and younger populations or have not been meaningfully reduced since statistics have been recorded.
Love Thy Neighbor:
There is something wonderful about many of the communities we live in. Our culture, with all of its flaws and idiosyncrasies, is an incredibly generous culture. We hear about suffering and hardship and our first instinct is to help. We raise money for countless causes and volunteer our time. The charitable nature of the American people is unparalleled in the world.
The closer to home the needs are the more we get involved. In my northern NJ community there is an organization called The Footprints In The Sand Foundation. They help families in their own community who have had tragedy or hardship to get through tough times. It could be as simple as bringing a family dinner for a week or so while they are trying to deal with a family crisis.
Receiving and offering help to and from your neighbors has a very powerful healing effect. It is common practice for neighbors to get together and provide meals for weeks and months to those in their communities who have to spend their days receiving radiation or chemotherapy, multiple invasive diagnostic tests etc. It is such a relief to not have to come home from an exhausting session of treatment, sometimes after a full day at work, and come home and have to prepare dinner for a family.
Are we helping or hurting?
I have one problem with our tradition of helping our neighbors. We may be interfering with their ability to heal. Now if you believe that healing from cancer is determined only by the drugs and radiation your doctors provide you, then this post will not mean much to you. However if you feel that the immune system (and that which controls the immune system) of the person is what does the healing and surgery, radiation and chemotherapy merely buys you time and perhaps can level the playing field a bit, then you want to give that immune system all the tools it needs to thrive and support health restoration.
My patients, who I am providing valuable information for about improving their “personal environment” as it relates to the food they eat, the air they breathe among other factors, are being given copious amounts of comfort foods by their well meaning neighbors at a time they are very vulnerable; during chemotherapy, radiation and recovery.
Allow me to be blunt:
One patient reports their family receiving trays of lasagna, pasta dishes, loaves of bread, cheeses and soft drinks. He reports that desserts, baked goods and sweets actually can exceed the amount of food provided for meals. Then there is the issue of the quantity of food. It is usually quantities that could feed a family 3 times the size and this goes on night after night. Here in the northeast, if you try to throw food away there is always that person in the family who says “no don’t throw the food away, it’s a sin”. Are you kidding, it’s a sin to kill yourself, and forcing yourself and family to eat food that is feeding cancer cells is insane.
Is comfort exactly what we should be providing?
There is another issue associated with the psychology of giving comfort. Going through a cancer diagnosis, all of the invasive dignity depleting procedures, exhausting and nauseating treatments is something I hope to never experience, but I am well aware of the toll it takes on the psyche of the patient and their family.
Sometimes you are just tired of thinking about healthy and unhealthy choices, maybe you want to flip the bird to anyone with an opinion about the choices you make, especially when your doctors don’t even stress the importance of these type of choices. If you’ve felt like “sh#@” for a month and have not been able to hold down a solid meal, then, now that you have your appetite back, someone is going to tell you ‘don’t eat lasagna, it has gluten, dairy, sugar, hormones, antibiotics’ You may just want to just to haul off and punch someone.
As a matter of fact if your oncology team is at a research facility, any step you take to improve your health is considered a confounding variable that interferes with outcomes in research related to drugs, radiation and chemotherapy, so the prevailing wisdom among the oncology research community is ‘don’t change a thing about your diet and lifestyle, let us do our job’.
I recognize this is a cynical view, but it happens to be true. I am not a cynical person by nature. I believe the people who choose to treat cancer are angels, sent by god to serve humanity and I do not question their integrity. They believe in what they do, as they should. However I have patients who have been to cancer treatment centers that are not research institutions, and every resource that has been shown to be helpful is utilized at the same time, including functional medicine, chiropractic, acupuncture, ayurveda etc. Each facility will choose to avail themselves of information that resonates with the prevailing mission of the institution. That can be very different from place to place. The decision to choose the right facility for you is a tough one.
The truth is, no one can tell you what you can and can’t eat. Once, being pissed off and frustrated no longer serves you, then you have to decide and ask yourself, “am I going to play a greater role in my healing? Am I going to take the time to learn more about how to make myself a healthier person, so I can assist my team in restoring my health, even if they try to talk me out of it.” You don’t have to become a doctor, but you can learn to become an expert in yourself and what type of environment will actually improve your health and immune function.
The choice to make a transition.
The choice to get involved and sort of swim upstream on the level of health restoration (not disease treatment. Disease treatment is your doctor’s job) is a choice only the patient can make. No one can do it for you. Once the decision is made and a shift occurs in your own heart and mind, the choices you can make no longer seem difficult, as a matter of fact they seem obvious. Anger, fear and frustration can begin to melt away on their own, you may even experience emotions like gratitude and optimism. Emotions like this can come out of nowhere.
People will appear in your life with pieces of the puzzle and provide you with abundant educational resources. Yes it can seem overwhelming and difficult to sift through, but it will get done. You’ll find that every decision you make is one that you feel more sure about and you can feel empowered and optimistic, an important milestone to reach.
Do not force the issue, take one step at a time by increasing your knowledge and seeking people in your life who will support you and take a break from the cynics and the negative people in your life.
Few would argue with the fact that our environment impacts our health and immune system. For those who read my posts, you heard me talk about your personal environment. Your personal environment includes what we allow to enter our body on a regular basis. What you breathe, eat and drink daily plays a big role in our ability to heal and restore our health.
Why pick on comfort food?
There is no shortage of information about how cancer can take hold in our body and actually thrive and grow. A lot of information that appears to be undeniable about the role sugar plays in cancer physiology. A direct extension of that is the fact that what we are talking about is not simply “table sugar” it is anything that our body responds to in the same way that it responds to table sugar. That includes:
- Alcohol
- Fruit
- Fruit juices
- Grains (including whole grains)
- Refined grain products like
- Pasta
- White rice
- Bread, muffins, other baked goods.
We could probably include and talk about foods with exogenous hormones, antibiotics, pesticides, herbicides and fungicides as being an additional source of stress for the already challenged immune system to deal with. For this post, let’s just stick to the sugars and perceived sugars.
Some of you reading this post might say, oh he is talking about staying away from carbs (carbohydrates). Well, yes and no. Vegetables are carbs, and I don’t want you to stay away from those as a matter of fact there are times of the year where your diet should be 70+% “carbs” from a vegetable source. There are times of the year I would encourage a greater intake of fruit (usually a brief period however, but that’s for another day). Of course there is a lot to know and learn. I believe your mindset as it relates to the above issues is a necessary hurdle before moving forward.
Foods and individual nutrients can be simply nutritious and they can be medicinal. Keep posted to this blog for more information about the role food and other environmental factors can impact our health and healing when experiencing diseases like cancer.
References:
- Warburg O. On the origin of cancer cells. Science 1956 Feb;123:309-14.
- Volk T, et al. pH in human tumor xenografts: effect of intravenous administration of glucose. Br J Cancer 1993 Sep;68(3):492-500.
- Digirolamo M. Diet and cancer: markers, prevention and treatment. New York: Plenum Press; 1994. p 203.
- Leeper DB, et al. Effect of i.v. glucose versus combined i.v. plus oral glucose on human tumor extracellular pH for potential sensitization to thermoradiotherapy. Int J Hyperthermia 1998 May-Jun;14(3):257-69.
- Rossi-Fanelli F, et al. Abnormal substrate metabolism and nutritional strategies in cancer management. JPEN J Parenter Enteral Nutr 1991 Nov-Dec;15(6):680-3.
- Brand-Miller J, et al. The glucose revolution. Newport (RI) Marlowe and Co.; 1999.
- Mooradian AD, et al. Glucotoxicity: potential mechanisms. Clin Geriatr Med 1999 May;15(2):
- Santisteban GA, et al. Glycemic modulation of tumor tolerance in a mouse model of breast cancer. Biochem Biophys Res Commun 1985 Nov 15;132(3):1174-9.
- Sanchez A, et al. Role of sugars in human neutrophilic phagocytosis. Am J Clin Nutr 1973 Nov;26(11):1180-84
- Moerman CJ, et al. Dietary sugar intake in the aetiology of biliary tract cancer. Int J Epidemiol 1993 Apr;22(2):207-14
- Seeley S. Diet and breast cancer: the possible connection with sugar consumption. Med Hypotheses 1983 Jul;11(3):319-27.
- Board M, et al. High Km glucose-phosphorylating (glucokinase) activities in a range of tumor cell lines and inhibition of rates of tumor growth by the specific enzyme inhibitor mannoheptulose. Cancer Res 1995 Aug 1;55(15):1178-85
- Gatenby RA. Potential role of FDG-PET imaging in understanding tumor-host interaction. J Nucl Med 1995 May;36(5):893-
Thanks for reading!





